In India, on average, more than 50,000 people daily donate blood. Blood donation is a Nobel thing that everyone should do once in their life. This is why knowing the complete details about blood donation, before donating the blood, will help us guide the complete ethical process of blood donation.
If you are a first-time blood donor and donŌĆÖt have any idea about blood donation, then you are at the very right place. Today, in this blog, we have added all the details about blood donation such as what blood donation is, its history, types of blood, types of blood donors, eligibility for donating blood, ineligibility, impact of blood donation on our health, and soon.
If you are also excited to know all these details about blood donation, then read this blog to the very end.
So, letŌĆÖs start-
Full Details about the Blood Donation
Blood donation in India is a vital, life-saving practice. This practice is supported by numerous organizations and government initiatives. Both Public and private sectors are consistently making aware the people about Blood donation but despite growing awareness, the country faces a recurring blood shortage. This is why, regular voluntary donations are crucial to meet the demand for safe blood. It will also ensure timely medical treatment for patients in need. We have added all the details about the blood donation in this blog below:
What is the blood donation?
Blood donation is a voluntary process where any individual or group of people donates their blood for ethical medical use. The donated blood is collected, tested, and stored in blood banks. It is ready to be used in transfusions for patients undergoing surgeries, treatment for chronic illnesses, or trauma care.
There are different types of blood donations: whole blood, platelets, plasma, and red blood cells, each serving specific medical needs. Donors are carefully screened to ensure their blood is safe for recipients. This altruistic act plays a crucial role in saving lives, maintaining public health, and supporting the healthcare system by ensuring a stable blood supply.
History of Blood Donation in India
The history of blood donation in India dates back to the early 20th century. The first recorded blood transfusion in India took place in 1939 at the Army Hospital in Pune. During World War II, the demand for blood transfusions increased. It led to the establishment of the first blood bank in India in 1942 in Kolkata, set up by Dr. Jivraj Mehta.
Post-independence, the Indian government recognized the importance of organized blood donation and transfusion services. The Indian Red Cross Society played a pivotal role in promoting voluntary blood donation. In 1962, the government established the National Blood Transfusion Council (NBTC) to oversee and regulate blood transfusion services across the country.
Different types of Blood / Classification of the Blood
Blood is a vital fluid in the human body, classified into different types based on various factors such as antigens and antibodies. The primary classifications are the ABO blood group system and the Rh factor, each playing a crucial role in blood transfusions, organ transplants, and medical diagnostics. Here’s a detailed overview of the different types of blood:
Compatibility of Blood Donation
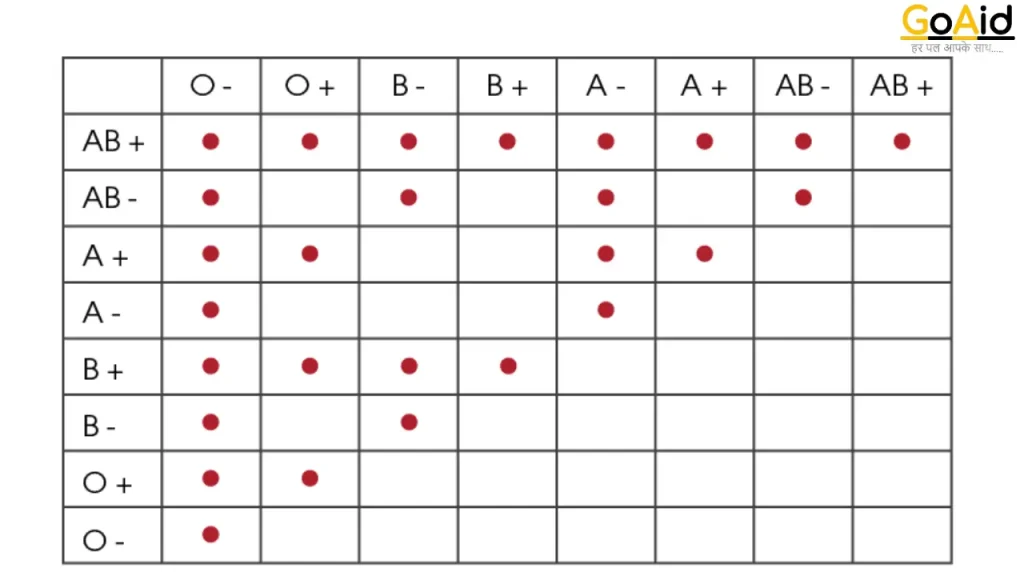
ABO Blood Group System
1. Type A
- Antigens: An antigen on the surface of red blood cells.
- Antibodies: Anti-B antibodies in the plasma.
- Subgroups: A1 and A2, with A1 being more common.
2. Type B
- Antigens: B antigens on the surface of red blood cells.
- Antibodies: Anti-A antibodies in the plasma.
3. Type AB
- Antigens: Both A and B antigens on the surface of red blood cells.
- Antibodies: No anti-A or anti-B antibodies in the plasma.
- Universal Recipient: Can receive blood from any ABO type.
4. Type O
- Antigens: No A or B antigens on the surface of red blood cells.
- Antibodies: Both anti-A and anti-B antibodies in the plasma.
- Universal Donor: Can donate blood to any ABO type.
Rh Factor (Rhesus Factor)
1. Rh-Positive (Rh+)
- Antigens: D antigen present on the surface of red blood cells.
- Compatibility: Can receive Rh+ and Rh- blood.
2. Rh-Negative (Rh-)
- Antigens: No D antigen on the surface of red blood cells.
- Compatibility: Can only receive Rh- blood.
Combined ABO and Rh Blood Types
Combining the ABO and Rh systems results in eight possible blood types:
- A+
- A-
- B+
- B-
- AB+
- AB-
- O+
- O-
Other Blood Group Systems
In addition to the ABO and Rh systems, there are other blood group systems, though less commonly referenced:
- Lewis System: Includes antigens such as Lea and Leb.
- Kell System: Includes antigens like K and k.
- Duffy System: Includes antigens Fya and Fyb.
- Kidd System: Includes antigens Jka and Jkb.
- MNS System: Includes antigens such as M, N, S, and s.
Importance of Blood Types
- Transfusion Safety: Ensuring compatibility to avoid adverse reactions.
- Pregnancy: Rh compatibility between mother and fetus to prevent hemolytic disease of the newborn.
- Organ Transplants: Matching donor and recipient blood types to reduce the risk of rejection.
Different Types of Blood Donor
Blood donors can be classified into different types based on their donation practices and the components of the blood they donate. Understanding these types helps in organizing blood donation drives and ensuring a steady supply of all necessary blood components. HereŌĆÖs a detailed overview of the different types of blood donors:
1. Voluntary Donor
Voluntary donors donate blood without any compensation, motivated purely by the desire to help others. This is considered the safest form of blood donation, as these donors are more likely to provide accurate health information and avoid risky behaviors that could affect the safety of the blood supply.
2. Replacement Donor
Replacement donors are individuals who donate blood to replace the blood used by a patient, often a friend or family member. This practice is common in some countries where there is a shortage of voluntary donors. Replacement donations help ensure that blood is available when needed, but it is not as reliable as a steady supply of voluntary donations.
3. Paid Donor
Paid donors receive compensation for donating blood. This practice is discouraged in many countries because it can lead to donors concealing health information, increasing the risk of blood-borne infections. The focus is on encouraging voluntary donations for a safer blood supply.
4. Autologous Donor
Autologous donors donate blood for their future use, often before undergoing surgery. This type of donation eliminates the risk of transfusion reactions and transmission of infections, as the donor is receiving their own blood.
5. Directed Donor
Directed donors donate blood specifically for a designated recipient, typically a family member or friend. While this can provide psychological comfort to the recipient, it is not necessarily safer than using blood from voluntary donors, as it still needs to be screened and tested.
Also Read: Sign of Heart Attack a Month Before
Types of Blood Donations
Whole Blood Donation
- Process: Donors give approximately one pint of whole blood.
- Use: The blood is typically separated into its components (red cells, plasma, platelets) for various medical uses.
- Frequency: Every 56 days (8 weeks).
Platelet Donation (Apheresis)
- Process: Platelets are collected using a machine that separates them from other blood components, returning the remaining blood to the donor.
- Use: Platelets are crucial for cancer patients, organ transplant recipients, and others with conditions affecting blood clotting.
- Frequency: Every 7 days, up to 24 times a year.
Plasma Donation (Apheresis)
- Process: Plasma is collected similarly to platelet donation, with blood components separated and returned to the donor.
- Use: Plasma is used for patients with liver conditions, burns, and severe infections.
- Frequency: Every 28 days, up to 13 times a year.
Double Red Cell Donation (Apheresis)
- Process: Two units of red blood cells are collected, and other components are returned to the donor.
- Use: Beneficial for trauma patients, those undergoing surgery, and individuals with severe anemia.
- Frequency: Every 112 days (16 weeks).
Special Donor Programs
- Universal Donors: Individuals with O-negative blood type are considered universal donors for red blood cells, as their blood can be transfused to patients of any blood type.
- Rare Donor Programs: Some donors have rare blood types or rare antigen combinations. Special programs maintain registries of these donors to ensure availability for patients with matching needs.
Eligibility Criteria for Blood Donation / Who can donate the Blood?
Eligibility criteria for blood donation in India are established to ensure the safety of both the donor and the recipient. These criteria can vary slightly between countries and organizations, but generally include the following guidelines:
Basic Eligibility Criteria
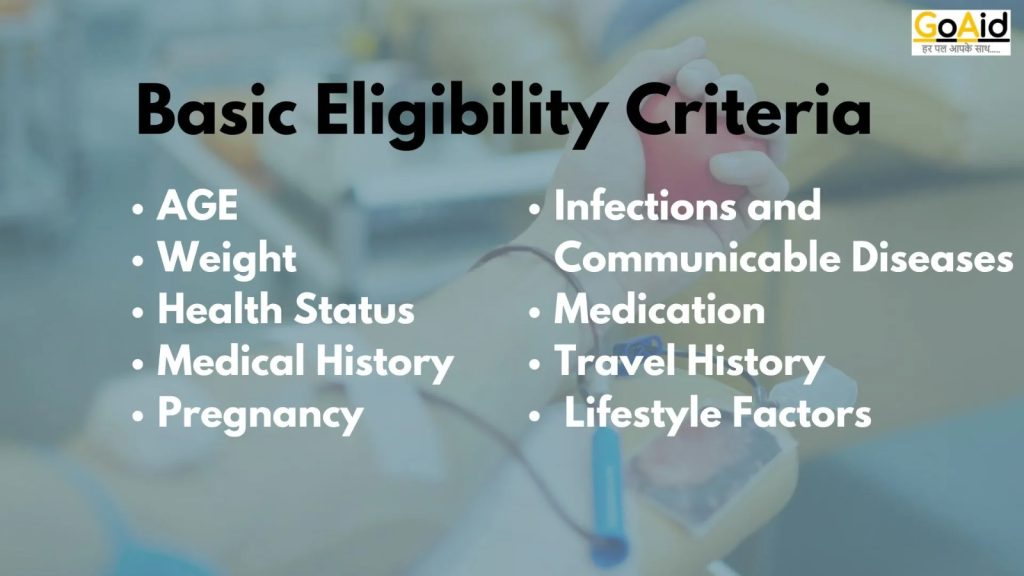
1. Age
- Donors must typically be between 18 and 65 years old.
- In some places, 17-year-olds may donate with parental consent, and older donors may be accepted if they meet health criteria.
2. Weight
- The minimum weight requirement is generally 50 kg (110 lbs).
- This ensures that the donor has sufficient blood volume to safely donate.
3. Health Status
- Donors should be in good general health at the time of donation.
- They must pass a basic physical examination, including checking blood pressure, pulse, temperature, and hemoglobin levels.
4. Medical History
- Donors must complete a detailed medical history questionnaire.
- Certain medical conditions (e.g., heart disease, cancer, severe anemia) and recent surgeries can disqualify a donor.
5. Infections and Communicable Diseases
- Donors must be free from infections and communicable diseases at the time of donation.
- Those with HIV/AIDS, hepatitis B and C, or syphilis are permanently deferred.
- Temporary deferrals may apply for recent infections, vaccinations, or certain travel histories.
6. Medication
- Some medications may disqualify a donor or require a temporary deferral.
- Donors should inform the screening personnel about all medications they are taking.
7. Travel History
- Recent travel to areas with a high risk of malaria, Zika virus, or other endemic diseases may result in a temporary deferral.
8. Lifestyle Factors
- Donors should not have engaged in high-risk behaviors such as intravenous drug use or unprotected sex with multiple partners.
- Recent tattoos or piercings may result in a temporary deferral (usually 6-12 months, depending on the location and regulations).
9. Pregnancy
- Pregnant women are not eligible to donate blood.
- Women must wait at least 6 weeks after childbirth to donate.
Specific Criteria for Different Types of Donations
1. Whole Blood Donation
- General eligibility criteria apply.
- Donors can donate every 56 days (8 weeks).
2. Platelet Donation (Apheresis)
- Donors may need to meet additional platelet count criteria.
- Platelet donors can donate more frequently, typically every 7 days, up to 24 times a year.
3. Plasma Donation (Apheresis)
- Similar health criteria as whole blood donors.
- Plasma donors can donate every 28 days, up to 13 times a year.
4. Double Red Cell Donation (Apheresis)
- Higher weight and hemoglobin requirements.
- Donors can donate every 112 days (16 weeks).
Ineligibility for Blood Donation / Who canŌĆÖt donate the Blood?
Well, the ineligibility of blood donation depends upon the type of blood donation event in which you are participating. But these are some of the most common ineligibilities of Blood Donation:
- Medical Conditions: Certain medical conditions may disqualify someone from donating blood. These conditions could include active infections, certain heart or lung conditions, blood disorders, certain cancers, and autoimmune diseases.
- Recent Surgery or Illness: People who have had surgery or been ill recently may need to wait until they have fully recovered before they can donate blood.
- Low Hemoglobin Levels: Blood donors must meet certain hemoglobin (iron) level requirements to ensure they can safely donate blood without risk to their health.
- Travel to Certain Countries: Travel to certain countries or regions may result in temporary deferral from blood donation due to the risk of exposure to infectious diseases such as malaria or variant Creutzfeldt-Jakob disease (vCJD).
- Recent Tattoos or Piercings: In some regions, individuals who have had tattoos or piercings within a certain timeframe may be temporarily ineligible to donate blood due to the risk of bloodborne infections.
- High-Risk Behaviors: People who engage in high-risk behaviors such as intravenous drug use or unprotected sexual activity with multiple partners may be ineligible to donate blood due to the increased risk of transmitting infectious diseases.
- Pregnancy or Recent Childbirth: Pregnant individuals or those who have recently given birth typically cannot donate blood until a certain period after childbirth.
- Certain Medications: Some medications may disqualify individuals from donating blood due to their potential effects on the recipient or the quality of the donated blood.
- Weight and Age Requirements: Blood donors typically need to meet minimum weight and age requirements to ensure their safety during the donation process.
- Health History and Lifestyle Factors: Individuals with a history of certain health conditions or lifestyle factors that could pose a risk to the donor or recipient may be ineligible to donate blood.
Expended ineligibilities for blood donation
Expended Ineligibility for blood donation is determined by several factors to ensure the safety and well-being of both the donor and the recipient. People who fall into the following categories are generally not eligible to donate blood:
Medical Conditions
1. Chronic Diseases
Individuals with chronic illnesses such as heart disease, lung disease, cancer, severe anemia, or uncontrolled diabetes are usually ineligible.
2. Infectious Diseases
Those with HIV/AIDS, hepatitis B or C, syphilis, and other sexually transmitted infections are permanently deferred.
Individuals who have had malaria in the past 3 years or have traveled to malaria-endemic areas recently may be temporarily deferred.
3. Severe Allergies
Persons with severe allergies that could be triggered by the donation process may be ineligible.
4. Autoimmune Disorders
Certain autoimmune diseases, such as lupus or multiple sclerosis, may disqualify a donor.
Recent Medical Procedures
1. Surgeries
Recent major surgeries typically require a deferral period, usually ranging from 6 to 12 months, depending on the surgery and recovery.
2. Transfusions
Recent recipients of blood transfusions are often deferred for a specific period, usually 12 months.
3. Vaccinations
Some vaccinations can lead to a temporary deferral, typically ranging from a few days to several weeks, depending on the type of vaccine.
4. Tattoos and Piercings
Individuals who have had tattoos or piercings within the last 6 to 12 months may be deferred, depending on the regulations and the sterility of the procedure.
Lifestyle Factors
2. High-Risk Behaviors
Individuals with a history of intravenous drug use, unprotected sex with multiple partners, or other high-risk behaviors are generally ineligible due to the increased risk of blood-borne infections.
2. Alcohol and Drug Use
Persons under the influence of alcohol or drugs at the time of donation cannot donate blood. Chronic substance abusers are also ineligible.
Specific Populations
1. Pregnancy and Breastfeeding
Pregnant women and those who are currently breastfeeding are not eligible. Women must wait at least 6 weeks after childbirth to donate.
2. Age and Weight
Those under the age of 18 or over the age of 65 (in some places) may be ineligible, though exceptions can sometimes be made for older donors in good health. Minimum weight requirements (typically 50 kg or 110 lbs) also apply.
3. Recent Illnesses
Individuals currently experiencing colds, flu, infections, or fever are temporarily deferred until they are fully recovered.
Certain Medications
Some medications may disqualify a donor temporarily or permanently. Donors must inform screening personnel about all medications they are taking, as some could affect the safety of the blood supply.
Blood and Bleeding Disorders
1. Hemophilia and Related Conditions
Individuals with bleeding disorders like hemophilia or those who take blood thinners are generally ineligible.
2. Other Blood Disorders
Conditions like sickle cell disease or thalassemia major may disqualify a donor, though those with sickle cell trait can often donate
The Benefits of Blood Donation
These are the Top 10 Benefits of the Blood Donation:
- Saving Lives: Perhaps the most significant benefit is the opportunity to save lives. Donated blood is used in various medical emergencies, surgeries, and treatments for patients with conditions such as cancer, anemia, and blood disorders.
- Supporting Medical Treatments: Blood transfusions are essential for patients undergoing surgeries, organ transplants, chemotherapy, and other medical treatments. Donors help ensure that these treatments can be carried out safely and effectively.
- Community Impact: Blood donation fosters a sense of community engagement and solidarity. By donating blood, individuals contribute to the well-being of their community and help support those in need.
- Cardiovascular Health: Regular blood donation has been linked to improved cardiovascular health. It helps lower iron levels in the body, reducing the risk of heart disease and improving blood circulation.
- Health Screening: The blood donation process involves a thorough health screening, which may help identify underlying health conditions such as high blood pressure, anemia, or infectious diseases. Donors receive feedback on their health status and may be prompted to seek further medical evaluation if needed.
- Stress Reduction: Donating blood has been associated with reduced stress levels. The act of giving and knowing that one is making a positive impact on someone else’s life can lead to feelings of satisfaction and fulfillment.
- Increased Iron Levels: For individuals with high iron levels, such as men and postmenopausal women, blood donation can help reduce excess iron stores. This can lower the risk of conditions like hemochromatosis, a disorder characterized by too much iron in the body.
- Regeneration of Blood Cells: The body replenishes the donated blood within a few weeks, leading to the production of new blood cells. This process helps maintain overall blood volume and ensures optimal oxygen delivery to tissues and organs.
- Weight Management: Donating blood may help in weight management for some individuals. The process burns approximately 650 calories for every pint of blood donated, which can contribute to calorie expenditure and weight loss over time.
- Long-Term Health Benefits: Studies suggest that regular blood donation may be associated with a lower risk of certain cancers, including liver, lung, and colon cancer. It may also reduce the risk of heart attacks and strokes by lowering blood viscosity.
Limit of Blood Donation in One Time
The limit of blood donation in one time refers to the maximum amount of blood an individual can safely donate during a single donation session. This limit is determined by various factors, including the donor’s health, weight, and the type of donation being made. Here are the complete details about the limits of blood donation at one time:
Whole Blood Donation
- Volume: The standard volume of whole blood collected during a donation is approximately 450 milliliters (mL), which is roughly equivalent to one US pint.
- Frequency: Donors can typically donate whole blood every 56 days (8 weeks), though this can vary depending on local regulations and the donor’s health status.
- Hemoglobin and Iron Levels: Donors’ hemoglobin levels are checked before each donation to ensure they are within the acceptable range. If a donor’s hemoglobin levels are too low, they may not be eligible to donate.
Platelet Donation (Apheresis)
- Volume: During a platelet donation (apheresis), a specific amount of platelets is collected based on the recipient’s needs, typically ranging from 200 to 500 milliliters.
- Frequency: Platelet donors can donate more frequently than whole blood donors, usually every 7 days, up to 24 times a year. However, the exact frequency may vary depending on local regulations and the donor’s platelet count.
Plasma Donation (Apheresis)
- Volume: Plasma donation involves the collection of plasma, which is the liquid portion of the blood, through a process called apheresis. The amount collected can vary but is typically around 600 to 800 milliliters.
- Frequency: Plasma donors can donate every 28 days, up to 13 times a year, though this may vary depending on local regulations and the donor’s health status.
Double Red Cell Donation (Apheresis)
- Volume: During a double red cell donation (apheresis), two units of red blood cells are collected, while the other components of the blood are returned to the donor. This results in a higher volume of blood being collected compared to whole blood donation, typically around 500 to 600 milliliters.
- Frequency: Double red cell donors can donate every 112 days (16 weeks), as this type of donation removes more red blood cells and takes longer for the body to replace.
Special Considerations
- Donor Health: The volume of blood collected in one donation is also influenced by the donor’s overall health, hydration status, and tolerance to the donation process.
- Regulatory Guidelines: Blood donation centers adhere to national and international regulatory guidelines that dictate the maximum allowable blood volume for donation at one time.
- Individual Variation: While there are general limits for blood donation at one time, individual variations may exist based on factors such as age, weight, and medical history.
Impact of Blood Donation on Our Health
There is both positive and negative impact of Blood Donation on our health:
Positive Impact of Blood Donation
- Improved Cardiovascular Health: Regular blood donation can reduce the risk of cardiovascular diseases by improving blood flow and lowering blood viscosity.
- Regeneration of Blood Cells: The body replenishes donated blood, leading to the production of new blood cells and enhancing overall blood circulation.
- Reduced Risk of Cancer: Some studies suggest that regular blood donation may lower the risk of certain cancers, including liver, lung, and colon cancer.
- Health Screening: Blood donation involves a thorough health screening process, which can help identify underlying health conditions such as high blood pressure, anemia, or infectious diseases.
Negative Impact of Blood Donation
- Temporary Fatigue: Some donors may experience temporary fatigue or weakness after donating blood, lasting from a few hours to a day. Adequate rest and hydration can help alleviate these symptoms.
- Iron Loss: Blood donation can lead to a temporary decrease in iron levels, especially in frequent donors or those with pre-existing iron deficiency. This may require supplementation or dietary adjustments.
- Bruising and Discomfort: Bruising or discomfort at the donation site is common and usually resolves within a few days. Applying ice and avoiding heavy lifting can help alleviate these symptoms.
- Fainting or Dizziness: Some donors may experience fainting or dizziness during or after donation, especially if they have low blood pressure or are sensitive to the sight of blood. Ensuring adequate hydration and eating a light meal before donation can help prevent these symptoms.
- Allergic Reactions: Rarely, donors may experience allergic reactions to the anticoagulant or other components used during the donation process. Prompt medical attention is necessary if severe allergic symptoms occur.
Diet After Blood Donation
These are some of the guidance about what or what types of meals you should have after bold donation. Maintaining a healthy diet after blood donation is crucial to support your body’s recovery and replenish the nutrients lost during the donation process. Here are some complete details about the diet after blood donation:
Hydration
- Water: Drink plenty of fluids, especially water, to help replenish the fluids lost during blood donation. Aim to drink at least 8-10 glasses of water throughout the day.
Nutrient-Rich Foods
- Iron-Rich Foods:
- Leafy Greens: Spinach, kale, and Swiss chard are excellent sources of iron.
- Lean Meats: Include poultry, fish, and lean cuts of beef or pork in your diet for heme iron, which is more easily absorbed by the body.
- Beans and Legumes: Lentils, chickpeas, and kidney beans are rich in non-heme iron, which is important for vegetarians and vegans.
- Fortified Foods: Choose iron-fortified cereals, bread, and pasta to boost your iron intake.
- Vitamin C-Rich Foods:
- Citrus Fruits: Oranges, grapefruits, lemons, and limes are high in vitamin C, which enhances iron absorption.
- Bell Peppers: Red, green, and yellow bell peppers are excellent sources of vitamin C.
- Berries: Strawberries, blueberries, raspberries, and blackberries are rich in vitamin C and antioxidants.
- Protein-Rich Foods:
- Eggs: Incorporate eggs into your diet for high-quality protein.
- Dairy Products: Choose low-fat dairy options like yogurt, milk, and cheese for protein and calcium.
- Nuts and Seeds: Almonds, walnuts, pumpkin seeds, and chia seeds are nutritious sources of protein and healthy fats.
- Folate-Rich Foods:
- Leafy Greens: Spinach, kale, and collard greens are rich in folate.
- Beans and Lentils: Incorporate beans, lentils, and chickpeas into your meals for folate and protein.
- Avocado: Avocados are a good source of folate and healthy fats.
General Dietary Guidelines
- Balanced Meals: Aim for balanced meals that include a combination of carbohydrates, proteins, and healthy fats.
- Frequent Meals: Eat smaller, more frequent meals throughout the day to maintain energy levels and prevent fatigue.
- Avoid Alcohol and Caffeine: Limit alcohol and caffeine consumption, as they can dehydrate the body and interfere with nutrient absorption.
- Limit Processed Foods: Minimize intake of processed foods, sugary snacks, and high-fat foods, as they provide little nutritional value and can contribute to weight gain.
Supplements
- Iron Supplements: If you have low iron levels or are at risk of developing iron deficiency, your healthcare provider may recommend iron supplements to support recovery.
- Multivitamins: Consider taking a multivitamin containing iron, vitamin C, and other essential nutrients to supplement your diet and support overall health.
10 Key Facts about the Blood Donation
These are the Top 10 Key Facts about Blood Donation:
- One Pint: During a typical blood donation, approximately one pint (about 470 milliliters) of blood is collected from the donor.
- Every Two Seconds: Someone in the United States needs blood every two seconds. This constant need emphasizes the importance of regular blood donations.
- Negative: Individuals with O negative blood type are considered universal donors because their blood can be transfused into patients with any blood type.
- AB Positive: Conversely, individuals with AB-positive blood type are universal recipients and can receive blood from donors of any blood type.
- Short Shelf Life: Red blood cells have a shelf life of up to 42 days, while platelets, crucial for clotting, have a shelf life of only 5 days. This short shelf life underscores the need for regular blood donations.
- Low Iron Levels: After donating blood, donors may experience a temporary decrease in iron levels, leading to feelings of fatigue or weakness. It’s important for donors to replenish their iron stores through diet and supplementation.
- Healthy Hearts: Regular blood donation can benefit the donor’s cardiovascular health by reducing the risk of heart disease. Donating blood lowers iron levels in the body, which can help prevent the buildup of excess iron linked to heart disease.
- World Blood Donor Day: June 14th is recognized as World Blood Donor Day, dedicated to raising awareness of the need for safe blood and blood products and thanking blood donors for their life-saving contributions.
- Voluntary Donors: Voluntary, unpaid donors are the safest source of blood. They are less likely to withhold medical information, leading to a safer blood supply for recipients.
- A Liter of Life: In some campaigns, it’s highlighted that one blood donation, approximately one pint, can save up to three lives when the blood is separated into its various components (red blood cells, platelets, and plasma) and used for different patients in need.
Also read: Diseases Caused in Rainy Season
Conclusion
In conclusion, blood donation in India encompasses a vital aspect of healthcare. It always relies on the active approach of donating blood of donors to save lives. Also, understanding who can donate, the benefits of donation, and the various types of donors underscores the significance of this act.
In this blog, we have added all the details about the blood donation with all aspects and details of the key points. We hope you have got the answer to all of your Queries in this blog. If you have any remaining queries, that you didnŌĆÖt find the answer to in our blog, please write that down in the comment box. We will resolve your query ASAP.
Thank you.
FAQs about the Blood Donation
┬ĀBlood donors can be categorized into various types, including voluntary donors, replacement donors, and directed donors. Voluntary donors donate blood willingly without expecting anything in return, while replacement donors give blood to replace blood used by a family member or friend. Directed donors donate blood specifically for a designated recipient, often for medical reasons such as compatibility concerns.
The amount of blood donated in one session depends on the type of donation and the donor’s health status. For whole blood donation, typically, about one pint (around 470 milliliters) of blood is collected. However, for platelet donation (apheresis), the donor’s platelets are separated from their blood, and the remaining components are returned to them, allowing for multiple donations during one session.
During a standard whole blood donation, approximately one pint (about 470 milliliters) of blood is collected from the donor. This amount is enough to make a significant impact and help save lives.
Certain individuals may be ineligible to donate blood due to medical reasons or lifestyle factors. Those with conditions such as HIV/AIDS, hepatitis B or C, and certain cancers are typically unable to donate. Additionally, individuals with low hemoglobin levels, recent surgeries, or high-risk behaviors such as intravenous drug use may be deferred from donating.
Blood donation is a vital practice that saves millions of lives worldwide each year. Did you know that one pint of donated blood can save up to three lives? Additionally, blood has a limited shelf life, with red blood cells lasting up to 42 days and platelets only 5 days, emphasizing the constant need for donations.
After donating blood, it’s essential to replenish nutrients and hydrate properly. Opt for iron-rich foods like leafy greens, lean meats, and beans to support red blood cell production. Additionally, consume foods high in vitamin C to enhance iron absorption and stay hydrated by drinking plenty of fluids, especially water.
Yes, blood donation can have health benefits for donors. It helps reduce the risk of cardiovascular diseases by lowering iron levels in the body, improves blood circulation, and may even lower the risk of certain cancers. Donating blood also promotes a sense of community engagement and satisfaction from helping others.
No, individuals experiencing cold, flu, or any other illness should refrain from donating blood until they have fully recovered. Donors must be in good health at the time of donation to ensure the safety of both the donor and the recipient.
The frequency of blood donation depends on the type of donation and the donor’s health status. For whole blood donation, donors can typically donate every 56 days (8 weeks), while platelet and plasma donors may be able to donate more frequently based on their platelet count and overall health.
Blood donation has numerous benefits, including saving lives, supporting medical treatments, improving cardiovascular health, and promoting community engagement. It also provides health benefits for donors, such as reducing the risk of heart disease, supporting weight management, and enhancing overall well-being.